Dr. Loor’s mission is to provide hope and cures for patients with advanced heart and lung disease through clinical excellence, research, leadership and education. Through his training and experience he has gained significant expertise in routine and complex adult cardiac surgery and is committed to quality improvement and best practices to make a positive difference in patients’ lives.
Show full bioDr. Loor is passionate about maximizing donor organs for lung transplant recipients given the high mortality of patients on the waitlist and a shortage of donor organs. He has successfully initiated portable ex vivo lung perfusion (EVLP) research and clinical programs and is credited with the first “breathing lung” transplant in the Midwest and in Texas.
Dr. Loor received his cardiac surgical and transplant training at Cleveland Clinic, after which he spent several years at the University of Minnesota as assistant professor in cardiac surgery, surgical director of the lung transplant program, co-director of the aortic program and co-director of the adult congenital program. There he significantly increased the volume and quality of lung transplantation through donor utilization and launched the acute aortic emergency program.
Presently, as surgical director of the lung transplant program at Baylor College of Medicine, Dr. Loor’s goal is to lead the world’s largest and highest quality lung transplant program. He also offers and supports the highest standards of clinical excellence and quality in cardiac surgery. Dr. Loor specializes in both routine and complex adult cardiac surgery as well as surgery for advanced heart and lung failure. He also participates in the interventional program for mitral valve and aortic valve disease where minimally invasive techniques are used to avoid open surgery. Dr. Loor’s research interests focus on improving donor utilization and surgical outcomes through basic and translational science collaborations and participation in outcomes registries and clinical trials. Dr. Loor chairs the Cardiovascular Quality Initiative group at Baylor St. Luke’s which seeks to optimize patient outcomes through multidisciplinary collaboration.
Texas Heart Institute Positions
- Teaching Staff, Thoracic Surgery Residency
- Editorial Board, Texas Heart Institute Journal
Current Projects
Interests
- Heart and Lung Transplant
- Pericardectomy
- Coronary artery bypass surgery
- Valvular heart disease
- Non-invasive mitral and aortic valve therapies
- Ventricular assist devices
- Pulmonary endarterectomy
- Cardiac tumors
Education
-
Undergraduate:
University of Miami (Biochemistry)
-
Medical School:
Northwestern University, Feinberg School of Medicine
-
Internship:
University of Chicago Hospitals
-
Residency:
University of Chicago Hospitals
Cleveland Clinic -
Fellowships:
University of Chicago Hospitals
Academic & Clinical Affiliations
- Baylor College of Medicine
- Baylor St. Luke's Medical Center
Certifications
- American Board of Thoracic Surgery
- American Board of Surgery
Publications
Recent News

Creative Strategies Used to Save COVID Patient Who Needed 149 Days of Extracorporeal Membrane Oxygenation
Infection with COVID-19 can take many forms. It can be mild enough to be mistaken for the common cold, or...

The Texas Heart Institute Journal’s Global Outreach
Since its founding in 1962, The Texas Heart Institute has remained dedicated to improving cardiovascular care worldwide through international collaboration,...
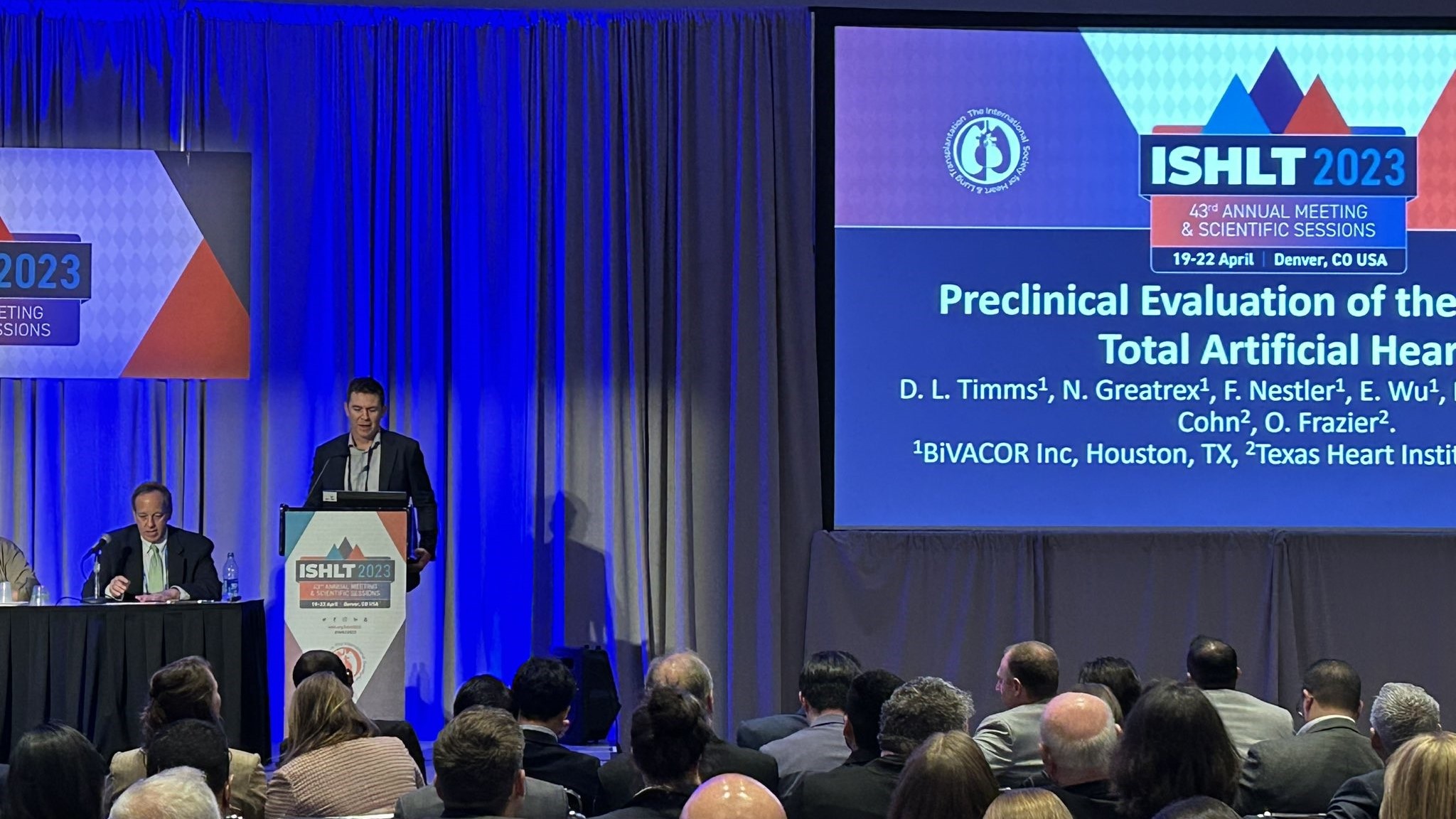
The Texas Heart Institute Makes a Strong Showing at ISHLT 2023
Daniel Timms, PhD, founder and chief technical officer of BiVACOR, Inc., described the benchtop testing and preclinical studies performed with...